
1. Which organs or tissues play a major role in managing our blood glucose levels?
When digested, the food produces glucose which is absorbed by the small intestine and further released into the blood. Once the glucose enters the blood, multiple organs and tissues play a significant role in regulating the blood glucose levels. The malfunctioning of any of these organs may result in fluctuations of blood sugar levels which may further lead to diabetes.
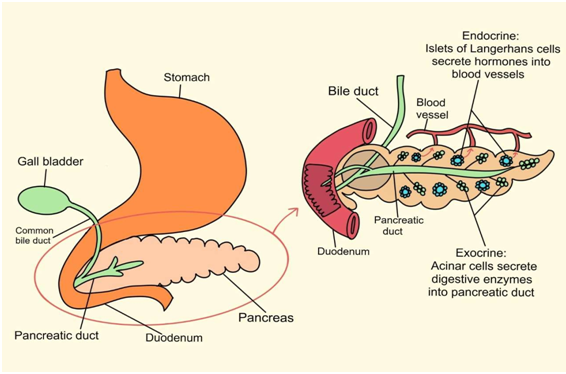
a. Pancreas is an organ located behind the lower part of the stomach. It has 2 portions. The exocrine part secretes digestive enzymes and helps in the digestion of food. The endocrine portion has cells called islets of Langerhans, which release hormones (chemical substances), namely glucagon and insulin, that manage our blood glucose levels. Insulin lowers blood sugar levels whereas glucagon increases blood glucose levels
Figure 1: Introduction to pancreas
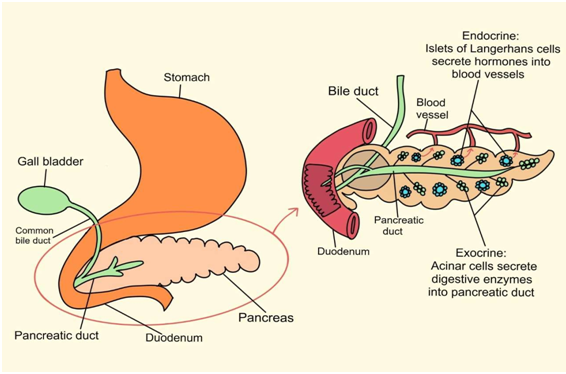
b. Muscles get energy from glucose to perform their functions. A muscle cell absorbs glucose from the blood with the help of insulin and stores it in the
 form of glycogen. It uses glucose and stored glycogen as and when required for energy and its function.
form of glycogen. It uses glucose and stored glycogen as and when required for energy and its function.c. Fat cells, also known as adipose tissues, absorb glucose from the blood with the help of insulin and store it as triglycerides (fat). It breaks down in starvation or when the body needs energy and releases free fatty acids (FFA).
d. Liver acts as the body's glucose reservoir as it stores and manufactures glucose from other components (like protein and fat) as and when required by the body. If glucose levels increase in the blood, it will absorb and store glucose. And, if glucose levels in the blood decrease, it makes glucose from other available components like protein and fat, and releases it into the blood. It is an essential organ in managing the glucose levels in the blood.
e. Brain uses glucose as its primary energy source, and it requires continuous delivery of glucose from the blood.
Therefore, tight control of blood glucose levels is essential for brain functioning. It also helps to manage blood glucose levels with the help of neuro-transmitors like GLUT 4 that signals islets of pancreas to release the hormones.
2. What are insulin and glucagon?
Insulin is a hormone (a chemical substance) produced by the beta cells of the Islets of Langerhans of the pancreas. It eases the entry of glucose and other substances into muscle, fat, and manages blood sugar levels.
Glucagon is a hormone (a chemical substance) produced by the alpha cells of the Islets of Langerhans of the pancreas. It acts opposite to insulin and helps to increase blood glucose levels by stimulating the liver to produce glucose and release it in blood.
3. Why is insulin needed in our body?
Insulin is essential to uphold the structure of our cells and tissues and stop them from breaking down in an uncontrolled manner. In other words, insulin keeps our cells and tissues well-nourished and healthy. Our tissues literally melt away into simple compounds without any insulin present and get excreted in the urine.
The 2 significant roles of insulin are:
1) Regulate blood sugar levels. After you eat, carbohydrates break down into glucose. Glucose then enters the bloodstream. The pancreas produces insulin, allowing glucose to enter the body's cells to provide energy. And in turn, keep a check on high sugar levels.
2) Store excess glucose for energy. After you eat, due to high glucose levels in the blood, the insulin helps to store the excess glucose in the liver in the form of glycogen and fat. When insulin levels are low, the liver releases glycogen and fat into the bloodstream in the form of glucose. This again helps to maintain blood glucose levels.
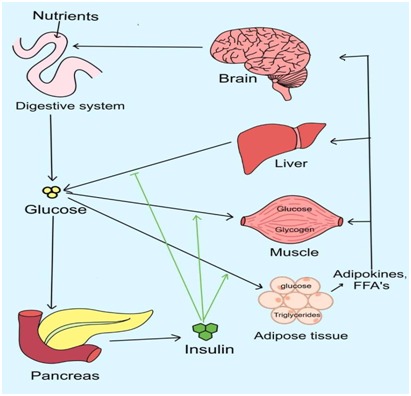
4. What is insulin resistance?
Insulin acts as a key to let the blood glucose into the cells. In the condition called insulin resistance, these cells stop responding to hormone insulin and the glucose can’t enter the cells. The three primary site for insulin resistance are liver, muscle and adipose tissues. Eventually, pancreas produces more insulin (hyperinsulinemia) to help glucose enter the cells. Even then, cells don’t recognize insulin and finally leads to rise in the blood glucose levels.
Figure 3: Role of insulin in glucose uptake by the cells

Insulin resistance leads to disorders like type 2 diabetes, gestational diabetes and pre-diabetes and many others.
5) Is insulin resistance different from diabetes?
Insulin resistance is the condition that eventually led to diabetes. When the cells can’t absorb glucose, sugar level builds up in the blood. If blood glucose is higher than the normal range, it is referred to as prediabetes.
Prediabetes often occurs in people with high insulin resistance. Thus, insulin resistance increases the risk of pre-diabetes and eventually diabetes.
People with insulin resistance produces more insulin to overcome body’s resistance towards insulin. Overtime, the beta cells of pancreas loses its ability to produce enough insulin leading to type 2 diabetes.
6. What causes insulin resistance?
The major factors causing insulin resistance are as follow:
● Excess weight – Too much of the fat around the abdomen area, a waist measurement of 40 inches (102 cm) or more in men and 35 inches (88cm) or more in women. A study has shown that visceral fat leads to long- lasting inflammation in the body.
● Ageing – Ageing leads to inflammation and in turn results in insulin resistance
● Excess intake of refined carbohydrates
● Lack of physical activity
● Inadequate sleep
● Genetic factors
● Chronic illness or inflammation
● Certain drugs like glucocorticoids
● Special conditions like pregnancy
7. What happens in hyperglycemia (high blood sugar levels)?
In diabetes and hyperglycemia (high blood glucose levels for a long time), one or the other organs/ tissues responsible for managing blood glucose start acting differently.
a. Small intestine may alter the secretion of gut hormones responsible for appetite, resulting in constant food intake and increased glucose levels. The decreased secretion of these hormones results in impaired insulin secretion and changes the gastric emptying and appetite control .
b. Muscles and fat cells may not uptake glucose due to either insulin deficiency or a condition called insulin resistance (see question 4). In turn, glucose remains in the blood, and the levels shoot up.
Figure 4: Blood glucose control mechanism in diabetes
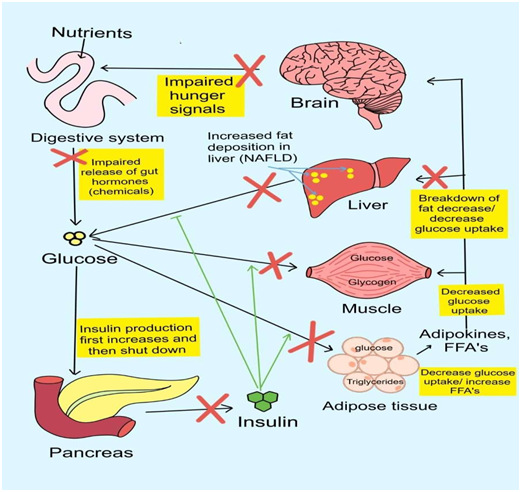
c. Pancreas initially compensates for high blood glucose by producing more insulin. This, in turn, also increases insulin levels in the blood, and the condition is termed hyperinsulinemia. This condition is the initial stage of type 2 diabetes. However, such prolonged demand and stress on beta cells leads to their death. By the time, 50% of beta cells are lost, type 2 diabetes ensues with high blood glucose levels.
d. Liver in individuals with type 2 diabetes, responds poorly to insulin, resulting in increased glycogen breakdown and increased production of glucose from non-carbohydrate sources. Once there is excess glucose in the blood and insulin resistance, it converts glucose into the fat and turns fatty liver. The condition is called non- alcoholic fatty liver disease [NAFLD]). This is prevalent is large group of people even without diabetes.
8. What is hypoglycemia? Isn't that opposite of diabetes?
Yes. Hypoglycemia (low blood sugar) is the opposite of hyperglycemia (high blood sugar), representing diabetes. Hypoglycemia is a condition in which blood glucose levels go lower than normal levels. It differs individually, but on average lower than 70mg/dl blood sugar levels indicate hypoglycemia in diabetes. If blood sugar levels become too low, signs and symptoms can include the following:
Figure 5: Symptoms of hypoglycemia

It occurs most commonly in people with diabetes. It is important to note that hypoglycemia is an early marker of diabetes and often occurs in people with pre-diabetes who are resistant to insulin, yet their pancreas produces enough insulin. After 3 to 5 hours of a meal, the blood glucose levels may fall rapidly, whereas the insulin levels may remain high. This may cause a temporarily lower level of blood glucose levels (hypoglycemia). Fortunately, it is treatable by providing instant glucose and changing the timings of the meals.
To read more on this topic, click here
